Surgery
The surgical part of our work involves not only the removal of painful teeth or roots that are not worth preserving, but in modern dentistry also includes bone augmentation and roots, surgical removal of inflamed bone areas while preserving the tooth (e.g. cyst removal or root tip resection, displaced teeth and tooth germ removal and also minor surgical mucosal procedures (cheek, tongue and lip ligaments). It also includes the surgical removal of inflamed bone areas while preserving the tooth (e.g. cyst removal or root tip resection), displaced teeth and tooth germ removal and also minor surgical mucosal interventions (cheek, tongue and lip ligaments), new mucosal formations (irritant fibromas, etc.), surgical gum treatment, roots with covering of bone pockets or gingivectomies, implant roots, transdental fixations (fixing and/or stabilization of loosened or too short roots), etc.

In our practice, most of the procedures are carried out by myself.
Would you like to know more? Take a look at “What do I have to consider before and after a surgical procedure?” or make an appointment with us for a consultation!
Extractions/tooth removal:
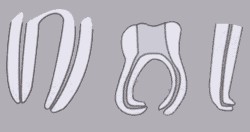
Removal of teeth by extraction
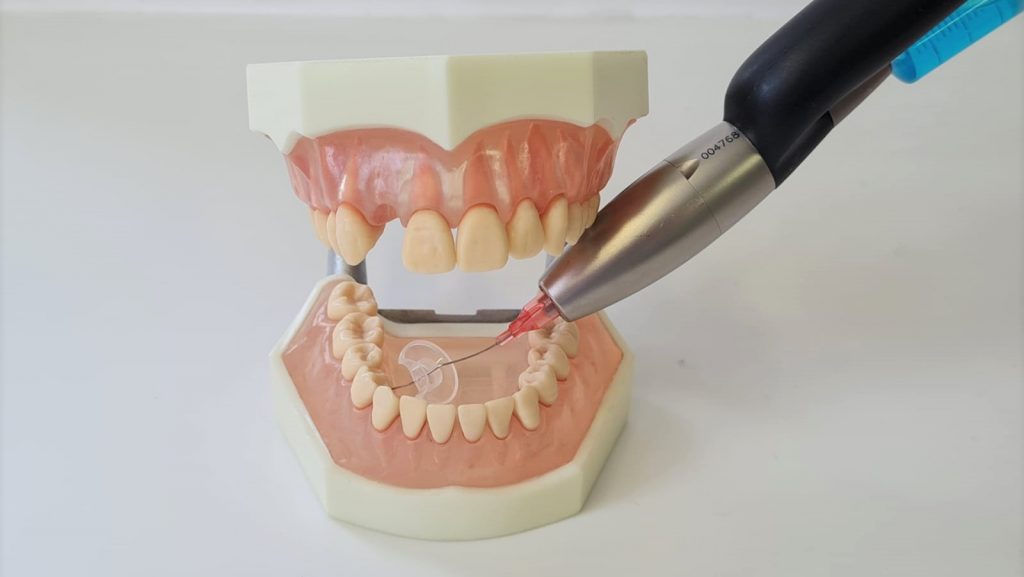
The removal of teeth or tooth roots that are no longer worth preserving is generally carried out under local anesthesia. With the help of certain instruments, the removal is carried out gently and with as little bone loss as possible (the bone is needed, for example, to be able to insert an implant later). Extractions are usually not carried out with force, but with certain techniques. If extraction complications arise, such a tooth may have to be surgically removed.
This service is covered by statutory health insurance.

What you should consider and know before undergoing dental surgery:
Please always inform us before such a procedure if there has been a change in your medication intake!
- Your appointment should be scheduled so that you can take your time and possibly come accompanied.
- The anesthetic may restrict your reaction speed afterwards – do not drive!
- You should take your usual medication and food.
- Risks that cannot always be ruled out:
◦ Wound healing disorders and wound infections
◦ Bruising, swelling and post-operative bleeding
◦ Intolerance reactions
◦ Possible closure of the wound by suturing over it
◦ Additional surgical intervention, e.g. if a tooth to be removed cannot be removed using the usual method (osteotomy)
◦ Involvement of surrounding tissue structures (maxillary sinus, nerves and blood vessels)
- If the maxillary sinus is involved, it is closed again in an extended procedure using a plastic cover.
- Nerve involvement, particularly in the lower jaw, can lead to numbness in the lip or tongue.
We will be happy to inform you about other side effects. Talk to us!
What you should consider and know -after- a dental surgical procedure:
- You should wait until the anesthetic is over before eating.
- Do not consume any hot drinks, do not smoke for at least 24 hours and do not consume any alcohol or other drinks that stimulate the circulation and thus promote post-operative bleeding.
- Do not drive a vehicle or participate in road traffic.
- The anesthetic may continue to work for 1-2 hours or longer.
- Please do not engage in any physical exertion, such as fitness training, over the next few days.
- Extensive but careful oral hygiene, no mouth baths for 24 hours so as not to jeopardize the forming blood clot (it is the plaster on the bone in your wound).
- If bleeding continues, bite firmly on a twisted handkerchief for approx. 20 minutes and also cool the facial area. If it continues to bleed, if you have severe pain for more than 1-2 days or if you develop a fever, contact us immediately.
- Take the medication prescribed by me punctually and regularly!
- The stitches are removed after 7-10 days.
Please be sure to come to your follow-up appointments, even if you are pain-free and feeling well!!!
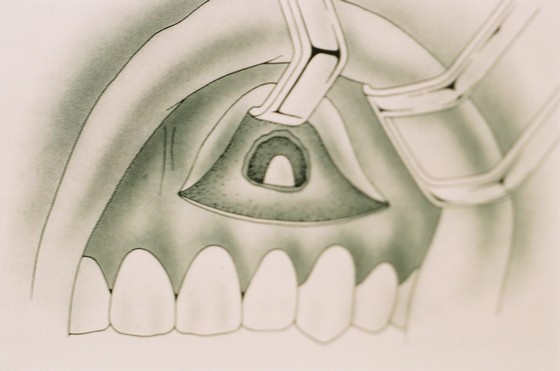
Removal of displaced teeth and tooth germs
Most displaced teeth or tooth germs are wisdom teeth that are tilted, rotated, impacted deep in the bone and often do not yet have fully developed root growth. We find the latter particularly in adolescents who come to us by referral, often for orthodontic treatment. Other displaced teeth are usually supernumerary teeth, such as double units, or displaced small molars that have not had room to fit straight into the jaw arch.
In rare cases, we also find an additional tooth. So-called pivot teeth are often hidden between the upper large incisors and cause a gap which does not close in the course of permanent tooth alignment (diasthema). These additional teeth are usually found as an incidental finding on an X-ray.
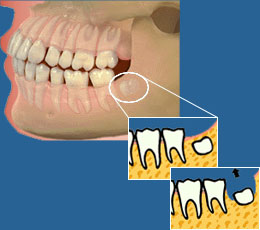


Removal of cysts
Cysts are fluid-filled cavities which, over time, represent a space-forming process at the expense of bone substance.
These are often so-called radicular cysts (originating from the root). These can be easily recognized on X-rays. The associated tooth is de-vital. It needs root canal treatment or already has a root filling. Sometimes a tooth that has had a root filling for years is also cracked, i.e. the root has a longitudinal fracture. Such a tooth is removed together with the cyst. Other root-filled teeth that are worth preserving are freed from their cysts by means of root tip resection.
With a few exceptions, your statutory health insurance will pay for this procedure.

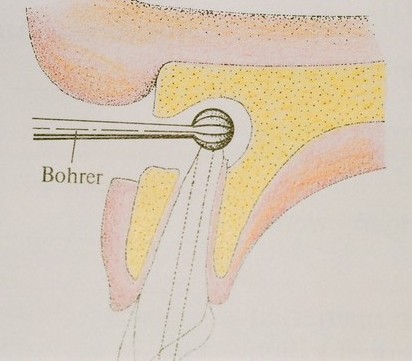
Root tip resections (WSR)
WSR is usually a minor and relatively quick surgical procedure in the upper or lower jaw.
The affected root is surgically exposed through a gum incision. The root tip is removed along with the inflammation. The area is then sutured well. For larger processes, the defect can be filled beforehand with bone substitute material and/or the patient’s own bone or membranes made from the patient’s own blood (PRF). These are also used to cover this area.
The area is irradiated with a laser after the operation to minimize soft tissue swelling and pain. The patient experiences hardly any discomfort as a result.
Your statutory health insurance will also pay for this procedure, except for the additional services. These will be discussed with you in advance and you will receive a private agreement.
Lip-/cheek-/tongue tie removal
These minor procedures affect the soft tissues and are usually without complications. They become necessary when the ligaments are too high and put too much pressure on the gum tips (papillae) between the teeth with every movement of the lips or tongue. If this is ignored for years, bone loss can occur at this point and the gums also recede in this area. This in turn can result in the need for another major soft tissue procedure. This is then a vestibuloplasty (deepening of the oral vestibule).

Oral vestibule deepening
This procedure restores the necessary distance between the movable and fixed gums, which should be at least 4 mm. This is particularly evident in very widely exposed tooth neck areas, often in the lower jaw anterior region, and once this distance has been restored, the bone in this area will not be reduced any further, at least for this reason.
Implantology
What is an implant?
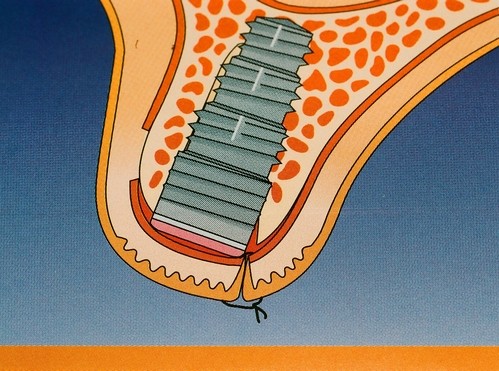
An implant is an artificial tooth root to replace your own missing teeth.
The surgical procedure is a private service (with a few exceptions defined by law).
Following the example of natural teeth, an implant is inserted into the jawbone onto which the denture is anchored once it has healed.
What are the benefits and advantages of an implant?
Grinding down the neighboring teeth and thus the loss of natural tooth material is avoided. Implants are used to augment abutments for free-end gaps to avoid removable clasp dentures. The prosthesis sits firmly, like your own teeth, and is also felt as such in the mouth. This restores confidence when communicating and eating and increases the quality of life enormously.
Another decisive advantage is that the artificially implanted roots prevent the jawbone from receding further at this point. In cases of complete edentulism, implants can help to restore a firm hold and perfect function to loose-fitting, removable dentures. This also guarantees safe communication with other people.


How is it done?
This is preceded by a planning phase, a consultation, X-rays of the jaw and a plaster model to analyze the implantation area.
In some cases, a DVT (digital volume tomography is a detailed diagnostic method with little X-ray radiation. The smallest bone structures of the skull can be depicted in three dimensions) in order to visualize anatomical structures such as nerves, maxillary sinuses or bone supply. The data set created is required to produce a template that shows the exact situation where the implant can be placed and how long or thick the implant should be. It helps to ensure that the implants can be positioned precisely. This makes it possible to transfer the implant planning exactly to the operation.
In exceptional cases, bone augmentation may also be necessary prior to implantation (with the patient’s own or artificial bone).
The implantation is usually performed under local anesthesia.
However, the surgical procedure can also be performed under twilight sedation at the patient’s request.
Special instruments are used to create an implant bed in the jaw that is the size of the implant to be inserted. The artificial titanium root is inserted into this, countersunk and closed with a small cover screw. Normally, such an implant heals in about six months in the upper jaw and about three months in the lower jaw before the implant post, which can be made of metal or ceramic and protrudes freely into the oral cavity, is inserted as a connecting piece to the denture after another small outpatient surgical procedure.


It is possible to rework existing dentures so that eating and speaking are guaranteed.
- A new temporary restoration is fabricated to ensure aesthetics, e.g. in the anterior region.
- A temporary restoration can also be dispensed with in the non-visible area.
There are only a few contraindications, such as systemic and some chronic diseases (e.g. poorly controlled diabetes mellitus, certain bone diseases, blood clotting and wound healing disorders). In the case of very severe nicotine abuse, drug or medication abuse, as well as specific mental illnesses and poor oral hygiene, my practice also refrains from implant surgery. These are risks that can lead to the loss of an implant even years later.
There are anatomical risks in the lower jaw due to the course of the supplying nerves, and in the upper jaw due to the proximity of the nasal and maxillary sinuses. For this reason, an adequate and comprehensive diagnosis must be made in advance.
However, there is always a residual risk!
Even with professional surgery, risks cannot always be ruled out, such as bruising, swelling, wound pain, opening of the maxillary sinus in the upper jaw, which is then immediately covered with plastic and thus closed again, numbness in the tongue and/or lip and cheek areas, taste impairments, which usually subside in the coming weeks, intolerance reactions to the anesthesia or nerve damage – also as a result of the anesthesia or other extremely rare risks.
Requirements for implantation
The most important prerequisite for an implant is a healthy periodontium, i.e. the gums must be healthy, which can be achieved through any previous gum treatment and professional tooth cleaning. The remaining dentition should also have been treated without caries prior to implant placement.
The bone must be sufficiently thick and high for the implant to be inserted. Otherwise, there are special treatment methods that can still be used to insert implants (e.g. bone splitting, internal and external sinus lift or bone replacement, which can be covered with membranes until final healing).
Permanent optimal oral hygiene is also necessary. This is monitored, improved and supported by recurring individual professional prophylaxis treatments following implantation and later after the definitive restoration.
WHY do I use titanium material in my practice?
Implants are exposed to high stresses during the chewing process. To ensure that they neither loosen nor twist over time, they must be firmly healed into the bone and form an intimate bond with it.
Titanium is electrochemically neutral, so that the bone cells react naturally and attach themselves closely to the implant surface. This gives the impression that they have grown into the bone.
Ceramic materials are still in the early stages of testing and further progress is needed before they are generally offered to patients in dental practices.
Implants have been around since the 1960s. A healed implant cannot easily break or loosen for no reason. According to long-term studies, the risk of loss over 10 years is around 5%, i.e. around 95% of implants inserted 10 years ago are still fully functional today.
The lifespan still depends on regular check-ups, individual oral hygiene, external influences, the correct loading of the implants and the patient’s state of health.
The cost depends on the number of implants, the implant system, the difficulty and the circumstances of the operation. For this reason, the financial scope is discussed with each patient in advance through extensive preliminary discussions.
As there are different implantation methods and forms of restoration, diagnostics, possible implant alternatives, the final prosthesis you expect and particular risks must be discussed in advance.
After the consultations, diagnostics and pre-treatment, each patient receives an individualized cost estimate from our practice, which includes all individually planned and foreseeable services.
The goal is a completely natural appearance with full and safe function of the chewing act and a natural feeling for the teeth.
Patients regain their confidence, which improves their quality of life and strengthens their psyche.
IF YOU HAVE ANY QUESTIONS, WE WILL BE HAPPY TO ADVISE YOU AND ARE AVAILABLE FOR A PERSONAL CONSULTATION!
INFO
Inserting implants into your jawbone is a surgical procedure. However, for many patients this is not as unpleasant as tooth removal.
It is important that you give us all the information about your state of health, especially any medication you are taking.
The anesthesia is usually performed under local anesthesia, i.e. you will receive an injection in the surgical area, making this area completely pain-free.
You should choose a convenient day for the operation, as you may have to miss work for a few days.
You will take all medication as usual (except for blood-thinning medication, which must be discussed with your general practitioner beforehand).
You should be picked up by an accompanying person, not actively participate in road traffic or carry out other responsible activities.
Come to your appointment well rested and early without stress.
Do not schedule any other important appointments in the coming days.
If circumstances permit, implant restorations can be fitted with immediate temporaries or existing dentures can be reworked without stress.
Sections of the jaw in the non-visible area should preferably remain without temporaries until final healing.
IF YOU HAVE ANY QUESTIONS, WE WILL BE HAPPY TO ADVISE YOU AND ARE AVAILABLE FOR A PERSONAL CONSULTATION!
The anesthetic is still in effect immediately after implantation. Your ability to react may therefore be limited and you should not actively participate in road traffic.
You should also refrain from responsible activities such as operating machinery etc. You should only eat and drink, especially hot food, when the numbness is no longer present so that you do not injure yourself unnoticed.
The implantation area must not be subjected to any stress for the next few days, as the implants need some time to integrate firmly into your bone. Therefore you should:
- not touch or suck on the wound,
- not carry out heavy physical work (certificate of incapacity for work, if applicable),
- Avoid alcohol, coffee, black tea, cola etc. and do not smoke,
- Avoid spicy food and very hot drinks,
- Perform physical therapy, such as cooling compresses (no heat),
- take all your prescribed medication punctually and regularly (e.g. antibiotics),
- not use mouthwashes on the first day, then use light mouthwashes with disinfectant mouthwashes,
- only brush carefully with a very soft toothbrush after a few days
- The sutures are removed after approx. 8 – 10 days.
- Any existing dentures must now be modified so that there is no load on the implant area, or you will receive a temporary denture.
IMPORTANT for long-term success:
- Regular and thorough oral hygiene to avoid bacterial plaque!
This is because bacterial plaque is partly responsible for inflammation of the gums surrounding the implant. This can lead to bone resorption and thus endanger the firmly healed implant (peri-implantitis).
Therefore:
- Brush your teeth for approx. 3 minutes after each meal and clean them with a disinfectant mouthwash; an electric toothbrush can optimize dental care (please consult Dr. Luther or your prophylaxis assistant),
- Floss or
 interdental brushes for cleaning the interdental spaces,
interdental brushes for cleaning the interdental spaces, - Toothpaste for the care of natural teeth,
- Regular check-up appointments and appointments for individual professional teeth cleaning by arrangement,
because of these controls
and your good oral hygiene, you can prevent pathological changes or detect and treat them in good time. In this way, you can help to protect yourself from complications!
IF YOU HAVE ANY QUESTIONS, WE WILL BE HAPPY TO ADVISE YOU AND ARE AVAILABLE FOR A PERSONAL CONSULTATION!
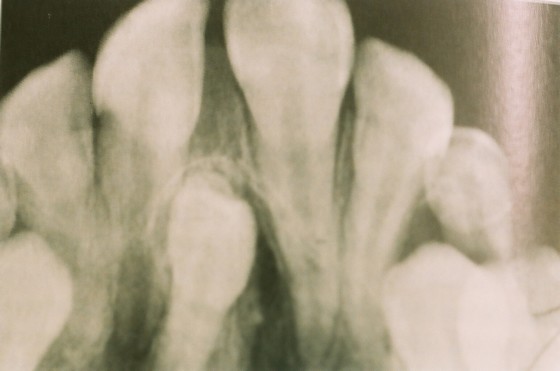
Root canal treatments
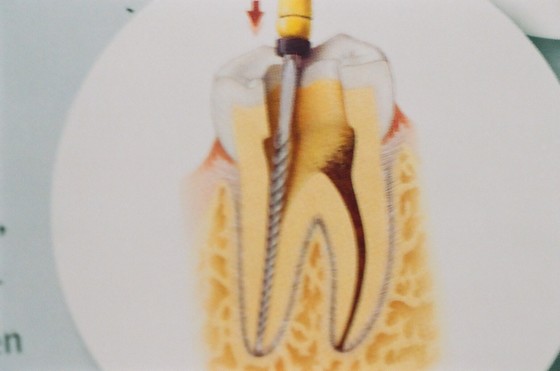
Every tooth is held in place by at least one root. The teeth are connected to the body via the root canal system through nerve tissue and blood vessels. A disease of this system often makes root canal treatment necessary.
The inflamed tissue must be removed so that the associated toothache can be eliminated and the tooth can be preserved.
Special fine preparation instruments are used to manually or mechanically clean the canal(s) of the inflamed tissue, rinse with disinfectant solutions, reduce the number of bacteria with laser treatment and then close the resulting cavity with a medical inlay or an appropriate root filling.
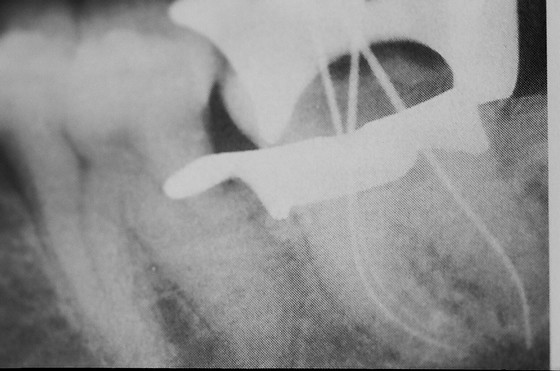
In between, it may be necessary to take X-rays to check the course of the canal and the degree of preparation. Electronic length measurements can help to reduce the number of x-rays.
Root canal treatments, which are particularly complex, difficult and time-consuming, are not always subject to the statutory health insurance guidelines, meaning that they are subject to private payment.
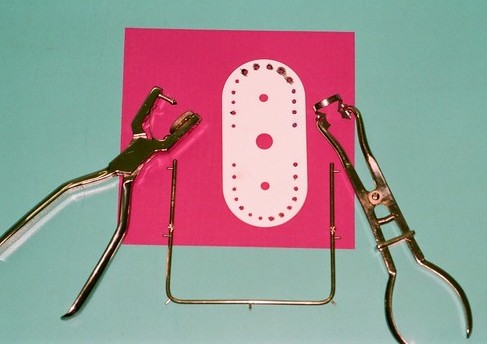
These treatments are carried out in my practice exclusively with magnifying glasses and appropriate bacteria-isolating measures (Cofferdam).
In our practice, after a detailed consultation, including possible alternatives, you will receive a private agreement in advance about the expected course of treatment and the expected costs.
IF YOU HAVE ANY QUESTIONS, WE WILL BE HAPPY TO ADVISE YOU AND ARE AVAILABLE FOR A PERSONAL CONSULTATION!




Root canal treatments, for particularly difficult cases
Root canal treatments are carried out when the tooth nerve is inflamed (pulpitis) or when nerve tissue is already dead.
Such an inflamed tooth can cause considerable pain and root canal treatment often has to be started unplanned. This involves removing the inflamed tissue.
The main cause is often pronounced caries, which infects the nerve through bacterial infiltration. This results in damage. Complicated anatomical conditions, particularly in the posterior molar region, often mean that these treatments are only possible outside the statutory health insurance guidelines. They are very time-consuming and extensive. Such teeth often have more root canals than expected. These can be found more easily with a magnifying glass and prepared using special methods. Particularly difficult anatomical conditions can also make the treatment very complex and time-consuming.
However, as the success of root canal treatment and thus the preservation of the teeth depends on the best possible preparation of the root canal areas up to the apex, it is often necessary to use special instruments. However, the small and fine lateral canals of the root cannot be reached. We often use the PACT device – photoactive therapy to minimize bacteria and the laser to dry the canals. In recent years, this has greatly reduced the amount of surgery (root tip resection) that often follows root filling.
Every tooth is supported by at least one root. The teeth are connected to the body via the root canal system through nerve tissue and blood vessels. Disease of this system often makes root canal treatment necessary.
The inflamed tissue must be removed in order to eliminate the associated toothache and preserve the tooth.
Special fine preparation instruments are used to manually or mechanically clean the canal(s) of the inflamed tissue, rinse with disinfectant solutions, reduce the number of bacteria with laser treatment and then close the resulting cavity with a medical inlay or an appropriate root canal filling.
In between, it may be necessary to take X-rays to check the course of the canal and the degree of preparation. Electronic length measurements can help to reduce the number of x-rays.
Root canal treatments, which are particularly complex, difficult and time-consuming, are not always subject to the statutory guidelines of the health insurance company, so that they are subject to private liquidation.
These treatments are carried out in my practice exclusively with magnifying glasses and appropriate bacteria-isolating measures.
In our practice, after a detailed consultation, including possible alternatives, you will receive a private agreement in advance about the expected course of treatment and the expected costs.



Laser, PACT
Laser: Lichtverstärkung durch stimulierte Emission von Strahlung
Special light waves are used in dentistry due to their physical properties. It is most frequently used to combat pathogenic bacteria during root canal and gum treatment, surgical procedures, caries diagnostics and much more.
Use:
- mainly in gum treatment, especially in the post-treatment phase
- for root canal treatments to dry the canal, seal lateral canals and reduce bacteria in the root canal
- to prevent swelling after operations (as a therapy laser)
- seals the tooth surface in the case of hypersensitive tooth necks
- for dentin germ reduction in ground teeth prior to the placement of dentures
- Treatment of herpes infections on the lips and aphthae in the oral cavity
- Quiet, gentle and painless treatment
The costs are not covered by statutory health insurance, but are sometimes covered by private health insurance.
IF YOU HAVE ANY QUESTIONS, WE WILL BE HAPPY TO ADVISE YOU AND ARE AVAILABLE FOR A PERSONAL CONSULTATION!

PACT: photodynamic therapy
It uses laser light to activate special dyes that kill pathogenic bacteria.
It is used in root canal treatment, for sterilization during implant treatment, after caries removal close to the tooth nerve, the pulp, for surface sterilization on prepared tooth stumps, before dental prostheses such as crowns or bridges are fitted, but also in the area of gum pocket treatment during periodontal treatment.


PRF
This is platelet-rich fibrin in autologous blood therapy. It can be produced in just a few minutes.
For larger processes, the defect can be filled beforehand with bone substitute material and/or the patient’s own bone or membranes made from the patient’s own blood (PRF). These are also used to cover this area to minimize soft tissue swelling and pain. Wound healing is optimized by PRF, especially in the soft tissue. The patient experiences hardly any discomfort as a result.
Use for: Extraction sockets, fresh bone wounds, after wisdom tooth surgery, for implantations, bone pocket therapy for PA problems,
PRF is used to cover bone defects in conjunction with the insertion of autologous or bone substitute materials in implantology or general dental surgery. It is a special procedure that requires the collection of venous blood, usually from the arm. This blood is separated into its components in a centrifuge using certain additives. Special components are then added back into the bone substitute.
The aim of PRF is to achieve faster healing, i.e. an increase in bone regeneration and natural bone growth/healing.
This service is purely private and does not necessarily have to be covered by private health insurance. You will receive a private agreement prior to the procedure.
IF YOU HAVE ANY QUESTIONS, WE WILL BE HAPPY TO ADVISE YOU AND ARE AVAILABLE FOR A PERSONAL CONSULTATION!

Advantages
PRF ...
- leads to better ossification
- leads to implant stabilization in bone resorption optimizes the regeneration of periodontal defects
- optimizes the regeneration of periodontal defects
- reduces the wound healing rate
- has a regenerative and reconstructive effect